Intrathecal Morphine Sulfate Injection: The Preferred Chronic Pain Treatment Option
May 5th, 2022 Drug, Patient, and Provider Safety, Education, Understanding Intrathecal Therapy
Using Oral Opioids for Chronic Pain Management
Understanding How Oral Opioids Work
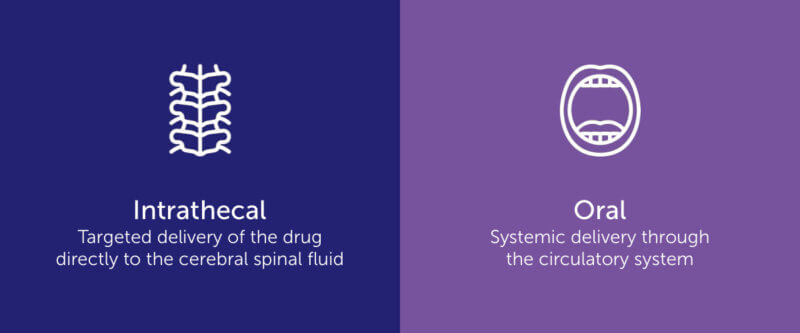
When initially diagnosed with chronic pain, a patient typically has one choice in terms of treatment: oral opioids.
Oral opioids are proven to be effective at mitigating chronic pain when prescribed and taken correctly. The keyword there being correctly. It’s important to understand how opioids work so patients know the risks and use their medications safely. Let’s take a deeper look at exactly how oral opioids work.
When a person takes a medicine, whether it’s morphine or acetaminophen or some other pill, it travels through the whole body, not just where it’s needed, before reaching the pain site. As it works its way through the esophagus, stomach, and intestines before finally getting into the bloodstream, the medicine breaks down, ultimately becoming less potent and effective. This, coupled with a patient’s increasing tolerance to the drug, is why a patient needs a stronger dose to get the same relief as time goes on. The dosage has to be continually adjusted, which can lead to some severe risks and side effects.
The Risks of Oral Opioid Use
It’s no secret that America continues to face an opioid crisis; the growth of which can largely be traced back to prescription painkillers. Morphine is highly addictive and when the dosage and treatment are not monitored by a healthcare professional misuse, abuse, addiction, and overuse may occur. Patients might think “I don’t need to talk to my doctor. I will just take more of what I have to ease the pain.” But, that can lead to a slippery slope. Of course, not every patient ends up an addict, but the risk is still very real.
Even for patients who don’t get addicted, there are other risk factors to oral opioids. Patients can experience adverse side effects including nausea, vomiting, constipation, pruritus, dizziness, dry mouth, sedation, and more. Doesn’t sound very pleasant, does it?
For chronic sufferers, dealing with pain is difficult enough. Why should healthcare providers make it more difficult by adding medication schedules and high risks? Luckily, there’s a safer, easier alternative – intrathecal therapy with morphine sulfate injection.
Morphine Sulfate Injection + Intrathecal Therapy = Better Pain Management Benefits
Better Control of Morphine Dosage and Use
Intrathecal therapy provides better control and measurement of morphine dosage and use. Whereas a patient taking oral medicine could ingest multiple pills at one time, the pump provides a measured, traceable dose. The patient can’t give themselves more medication than the pump is programmed to release and the reservoir only holds a certain amount of morphine sulfate at any given time. Thus, the chances of drug misuse or overuse significantly decrease.
Not only is the risk of abuse decreased, but the amount of medication needed is lower when using intrathecal therapy. Because of its targeted delivery method, intrathecal injectable morphine sulfate doesn’t break down like oral opioids. The intrathecal medication is just as potent when it reaches the pain site as it was when it entered the pump, meaning the patient gets stronger relief with a fraction of the amount of an oral dose. It also means there is less dosage escalation over time.
Less Adverse Side Effects
The risk of experiencing adverse side effects also decreases with the use of intrathecal therapy. While some side effects may still occur, continuous dosing with a morphine sulfate pump lessens the most common and harshest reactions.
Safer to Administer
Intrathecal therapy isn’t just safer for patients but can provide benefits to providers as well. When choosing which morphine sulfate injection option to use, providers should consider MITIGO™.
Why choose MITIGO over other injectable morphine options?
- As the only FDA-approved injectable morphine to come packaged in a vial, MITIGO removes the need to break glass ampules, thus removing the risk of injury or bacterial contamination due to broken glass.
- It’s easier to draw medication from a vial than a glass ampule which results in less drug waste.
- The non-compounded formula means there’s no mixing required before administering. Providers don’t have to worry about the patient receiving a variance in potency.
- Pump manufacturers prefer the use of non-compounded drugs as they don’t clog the device. Choosing MITIGO allows for longer pump use and a higher probability of insurance coverage.
- As a non-compounded drug, MITIGO’s potency has proven stable throughout its shelf life, unlike compounded drugs.
- Non-compounded drugs have a longer shelf life than compounded drugs, helping to reduce drug waste.
- With access to Piramal Critical Care’s dedicated team and educational programs, providers are up-to-date on the latest news and training to ensure they’re keeping themselves and their patients safe.
Healthcare providers always want what’s best for their patients, but when what’s best for the patient is also what’s best for the provider, it’s a win-win!
Making the Switch to Intrathecal Therapy
After considering the risks of oral opioid use and seeing the benefits of morphine sulfate injection through intrathecal therapy, the choice of which treatment to choose seems obvious. Morphine sulfate injection delivers better, more controlled results than oral opioids but it is still an opioid and needs to be monitored by a medical professional.
If you’re a patient looking to move from oral to intrathecal treatment, work with your medical team to discover the best path forward.
If you’re a medical or healthcare provider and are interested in learning more about MITIGO, sign up for one of our education programs or contact us to book a meeting with our team.
Contact us for more information on MITIGO
Important Risk Information
INDICATIONS AND USAGE
MITIGO™ (Morphine Sulfate Injection, USP – Preservative-free) is an opioid agonist, for use in continuous microinfusion devices and indicated only for intrathecal or epidural infusion in the management of intractable chronic pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.
IMPORTANT RISK INFORMATION
WARNING: RISKS WITH NEURAXIAL ADMINISTRATION; LIFE-THREATENING RESPIRATORY DEPRESSION; RISK OF ADDICTION, ABUSE, AND MISUSE; NEONATAL OPIOID WITHDRAWAL SYNDROME; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
See full prescribing information for complete boxed warning.
- Single-dose neuraxial administration may result in acute or delayed respiratory depression up to 24 hours. Because of the risk of severe adverse reactions when MITIGO is administered by the epidural or intrathecal route of administration, patients must be observed in a fully equipped and staffed environment for at least 24 hours after the initial dose.
- Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Patients must be observed in a fully equipped and staffed environment for at least 24 hours after each test dose and, as indicated, for the first several days after surgery.
- MITIGO exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient’s risk before prescribing and monitor regularly for these behaviors and conditions.
- Prolonged use of MITIGO during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
- Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate; limit dosages and durations to the minimum required; and follow patients for signs and symptoms of respiratory depression and sedation.
CONTRAINDICATIONS
- Significant respiratory depression
- Acute or severe bronchial asthma in an unmonitored setting in absence of resuscitative equipment
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days
- Known or suspected gastrointestinal obstruction, including paralytic ileus
- Hypersensitivity or intolerance to morphine
Neuraxial administration of MITIGO is contraindicated in patients with:
- Infection at the injection microinfusion site
- Concomitant anticoagulant therapy
- Uncontrolled bleeding diathesis
- The presence of any other concomitant therapy or medical condition which would render epidural or intrathecal administration of medication especially hazardous.
WARNINGS AND PRECAUTIONS
- Risk of Inflammatory Masses: Monitor patients receiving continuous infusion of MITIGO via indwelling intrathecal catheter for new signs or symptoms of neurologic impairment.
- Risk of Tolerance and Myoclonic Activity: Monitor patients for unusual acceleration of neuraxial morphine, which may cause myoclonic-like spasm of lower extremities. Detoxification may be required.
- Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients: Monitor closely, particularly during initiation and titration.
- Adrenal Insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid.
- Severe Hypotension: Monitor during dosage initiation and titration. Avoid use of MITIGO in patients with circulatory shock.
- Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness: Monitor for sedation and respiratory depression. Avoid use of MITIGO in patients with impaired consciousness or coma.
ADVERSE REACTIONS
Most serious adverse reactions were respiratory depression, apnea, circulatory depression, respiratory arrest, shock, and cardiac arrest. Other common frequently observed adverse reactions include: sedation, lightheadedness, dizziness, nausea, vomiting, and constipation.
USE IN SPECIFIC POPULATIONS
- Pregnancy: May cause fetal harm.
- Hepatic and Renal Impairment: May affect the metabolism and excretion of MITIGO.
To report SUSPECTED ADVERSE REACTIONS, contact Piramal Critical Care, Inc. at 1-888-822-8431 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
For additional Important Risk Information, including boxed warning, see enclosed Full Prescribing Information.
INDICATIONS AND USAGE
MITIGO™ (Morphine Sulfate Injection, USP – Preservative-free) is an opioid agonist, for use in continuous microinfusion devices and indicated only for intrathecal or epidural infusion in the management of intractable chronic pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.
IMPORTANT RISK INFORMATION
WARNING: RISKS WITH NEURAXIAL ADMINISTRATION; LIFE-THREATENING RESPIRATORY DEPRESSION; RISK OF ADDICTION, ABUSE, AND MISUSE; NEONATAL OPIOID WITHDRAWAL SYNDROME; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
See full prescribing information for complete boxed warning.
- Single-dose neuraxial administration may result in acute or delayed respiratory depression up to 24 hours. Because of the risk of severe adverse reactions when MITIGO is administered by the epidural or intrathecal route of administration, patients must be observed in a fully equipped and staffed environment for at least 24 hours after the initial dose.
- Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Patients must be observed in a fully equipped and staffed environment for at least 24 hours after each test dose and, as indicated, for the first several days after surgery.
- MITIGO exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient’s risk before prescribing and monitor regularly for these behaviors and conditions.
- Prolonged use of MITIGO during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
- Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate; limit dosages and durations to the minimum required; and follow patients for signs and symptoms of respiratory depression and sedation.
CONTRAINDICATIONS
- Significant respiratory depression
- Acute or severe bronchial asthma in an unmonitored setting in absence of resuscitative equipment
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days
- Known or suspected gastrointestinal obstruction, including paralytic ileus
- Hypersensitivity or intolerance to morphine
Neuraxial administration of MITIGO is contraindicated in patients with:
- Infection at the injection microinfusion site
- Concomitant anticoagulant therapy
- Uncontrolled bleeding diathesis
- The presence of any other concomitant therapy or medical condition which would render epidural or intrathecal administration of medication especially hazardous.
WARNINGS AND PRECAUTIONS
- Risk of Inflammatory Masses: Monitor patients receiving continuous infusion of MITIGO via indwelling intrathecal catheter for new signs or symptoms of neurologic impairment.
- Risk of Tolerance and Myoclonic Activity: Monitor patients for unusual acceleration of neuraxial morphine, which may cause myoclonic-like spasm of lower extremities. Detoxification may be required.
- Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients: Monitor closely, particularly during initiation and titration.
- Adrenal Insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid.
- Severe Hypotension: Monitor during dosage initiation and titration. Avoid use of MITIGO in patients with circulatory shock.
- Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness: Monitor for sedation and respiratory depression. Avoid use of MITIGO in patients with impaired consciousness or coma.
ADVERSE REACTIONS
Most serious adverse reactions were respiratory depression, apnea, circulatory depression, respiratory arrest, shock, and cardiac arrest. Other common frequently observed adverse reactions include: sedation, lightheadedness, dizziness, nausea, vomiting, and constipation.
USE IN SPECIFIC POPULATIONS
- Pregnancy: May cause fetal harm.
- Hepatic and Renal Impairment: May affect the metabolism and excretion of MITIGO.
To report SUSPECTED ADVERSE REACTIONS, contact Piramal Critical Care, Inc. at 1-888-822-8431 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
For additional Important Risk Information, including boxed warning, see enclosed Full Prescribing Information.